My therapy options

Which therapy option is right for me?
Your physician has discussed with you that your kidney function is severely impaired and that you will soon need to select a Renal Replacement Therapy (RRT) option that is the most suitable for you, to preserve both your life and quality of life. As there is more than one therapy option available for many patients, it is important that you take the opportunity to learn more about your therapy options to make the right choice for you personally.
Choosing the right therapy for kidney failure may be difficult. Become familiar with the therapy options and, together with your physician, choose the therapy that best suits your health status and lifestyle.
The dialysis therapy you chose is not set in stone. Your personal lifestyle and changing medical factors also play a role in your choice of therapy. Those factors may change during your life or there might be complications which require switching to another form of treatment. Many patients do not undergo just one form of treatment in their lifetimes.
Each therapy option has its own advantages and disadvantages and not every therapy is suitable for every patient, which may limit your choices. Together with your physician and your family, you can decide which therapy is best for you in terms of treatment results and your individual quality of life.

Supporting you on your way
We would like to support you on your path to the right therapy and have compiled the most important information about different therapy options.
- With some tips that support choosing the right therapy, we will provide you some guidance on the way to making a decision
- We want to introduce to you the most important therapy options:
transplantation, peritoneal dialysis, haemodialysis, home haemodialysis and conservative therapy
- The dialysis therapy you chose is not set in stone…
- Dialysis changes your everyday life. In the section My life with dialysis, we address the most relevant topics for choosing a therapy option: everyday life, exercising, holidays and nutrition
Kidney transplantation
A kidney transplant is the transfer of a healthy kidney from a donor into a patient (recipient) with chronic kidney failure.
Whether a patient (recipient) is suitable for a kidney transplant depends on various medical considerations. Different laboratory tests are done to make sure that the donor kidney and the recipient are a match.
The time it takes to receive a donor kidney varies greatly. Unfortunately, there are not enough kidneys available for transplantation. For this reason, patients may often be on a waiting list for a long time.
Who can donate a kidney?
- A living blood relative (e.g. parents or siblings).
- A living unrelated donor (e.g. a life partner or very close friend)
- A deceased donor
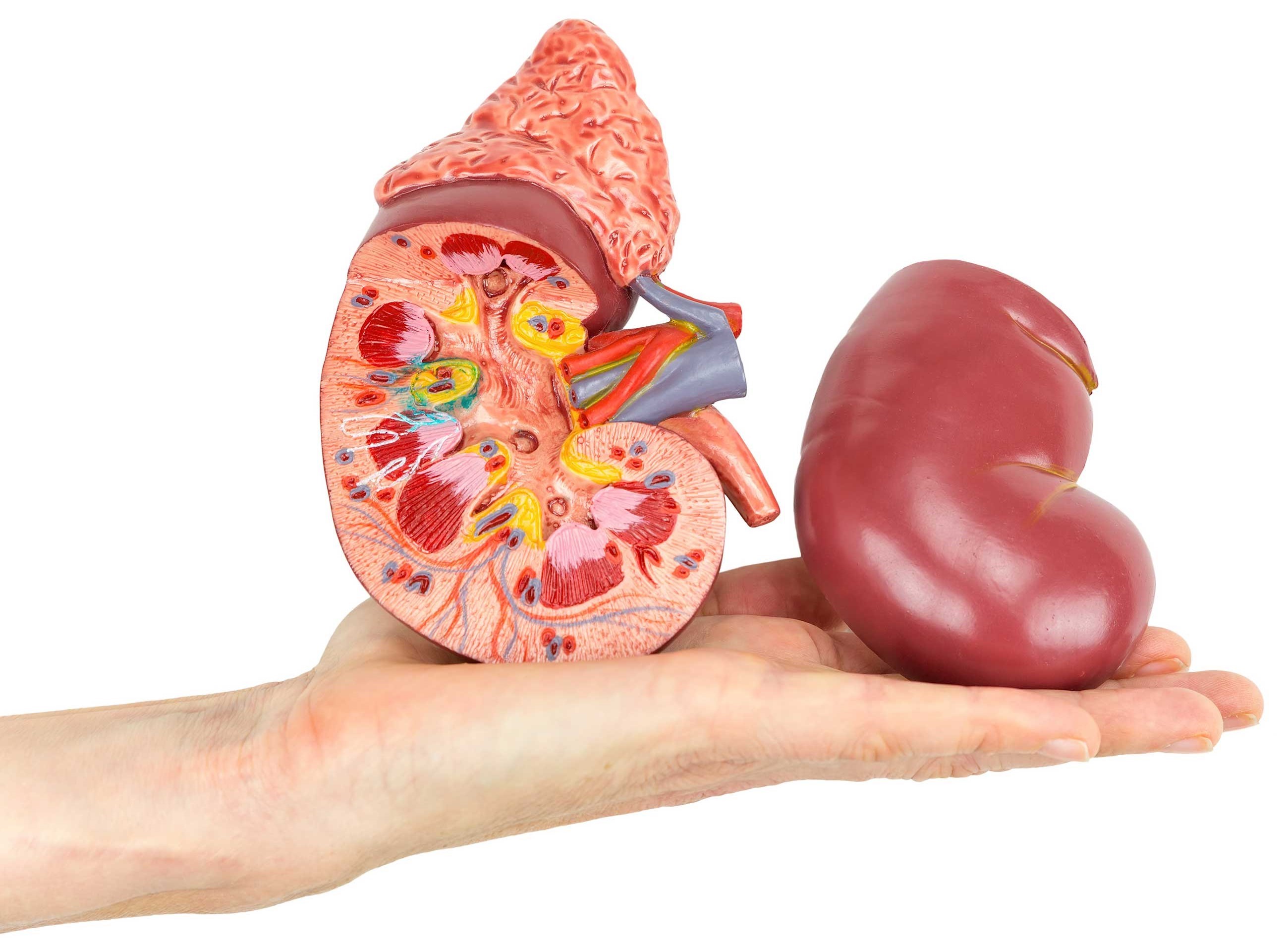
How does a kidney transplant work?
The donor kidney is inserted into the lower parts of the abdomen. The diseased kidneys are usually not removed, mainly so patients benefit from the remaining functions of the kidney. If all goes well (i.e. the surgery is successful and appropriate medication to keep the kidney within the body and prevent rejection), the new kidney takes over the tasks of the diseased kidneys enough to partially restore the lost kidney function. A successfully transplanted kidney can work for many years. If the transplant is not successful, dialysis is still an option. Many patients with kidney disease go through different treatment modalities during their lifetimes (e.g. starting with peritoneal dialysis, then a having kidney transplant, then switching to haemodialysis after the donor kidney may lose function or complications occur), so a failed transplant is not the last option.
What needs to be considered for a kidney transplant?
A successful transplant can help the patient to achieve a better state of health without dialysis. To prevent rejection of the donor kidney, the patient (recipient) must take regular medications during and/or after the transplant. These medications are generally referred to as immunosuppressives.
Since your immune system will be weaker compared to that of others, you should be aware of the potential complications of immunosupressive therapy i.e. risk of developing infections. Therefore, it is essential to follow advice given by your healthcare team. These medications can cause side effects, which may vary depending on the type of immunosupressants. You will be monitored for these, and given advice on how to look out for some of these complications. For patients with a donor kidney, it is important that the anti-rejection and other medication is taken daily and that regular follow-up examinations take place.
Peritoneal Dialysis (PD)
Peritoneal Dialysis (PD) is named after the peritoneum. This is a thin, velvety tissue that lines the abdominal cavity and the internal organs. It is naturally present in every person’s body. This form of dialysis uses the peritoneum as a natural filter to replace kidney function. To do so, a fresh dialysis solution is introduced into the abdomen via a soft tube called a catheter that is surgically inserted into your abdomen. Depending on your physician’s prescription, it remains there for a few hours and is replaced as soon as toxins and excess body water have been absorbed.
The PD catheter
- A catheter is a soft, flexible plastic tube that is about the width of a straw in diameter.
- In peritoneal dialysis, dialysis fluid flows in or out of the abdomen through the catheter.
- The catheter is placed into the abdominal cavity through a minor surgical procedure and permanently remains in place. It is usually ready for use two weeks after the surgery.
There are two types of PD
PD is performed either as Continuous Ambulatory Peritoneal Dialysis (CAPD) (manually) or as Automated Peritoneal Dialysis (APD) (using a machine). In rare cases, a combination of two types can also be used. PD treatment is performed by filling the abdomen with dialysate (these are called exchanges), allowing the dialysate to remain for a prescribed dwell time, then draining the waste fluid from the abdomen. Excellent standards of hygiene are mandatory for PD treatment to avoid risk of infection and you must take great care to protect your exit site. There is time whilst on PD treatment for you to participate in seated activities such as reading a book. You will receive extensive training from your care team before performing dialysis on your own, all necessary steps will be communicated during training. The decision to use one of the two PD options depends on your lifestyle, health condition and personal preferences and is made together in consultation with your physician. You may find it helpful to involve relatives or other patients in your decision. Everything can be done together!
Facts about PD
- You perform the treatment independently, seven days a week, at home, as prescribed by your nephrologist.
- However, you are not alone: a physician will check on you regularly and a PD nurse is available for you on-call by phone.
- With PD, you are relatively flexible. That allows you to plan your daily life. This can be important for you if you work, go to school or travel.
What you need to do to succeed at PD:
- You will receive detailed training at your dialysis centre to ensure that you feel comfortable doing PD on your own. You will also learn proper catheter care.
- Be aware that it may take some time to get used to the fluid in your stomach. It is usually not a problem for an adult to have two to three litres of fluid in their abdominal cavity.
- Following certain precautions will help you avoid the risk of an infection called peritonitis. Hygiene control is one of the most critical aspects of PD therapy. Your nurse will give you instructions on how to avoid infection.
- You will need ample storage space for your supplies at home.
- If you have diabetes, be aware that your physician may need to adjust your dose of diabetes medications. This is because the sugar in the dialysis fluid may raise your blood sugar levels.
- You will perform your treatment every day, seven days a week, as prescribed by your nephrologist.
- You will visit your dialysis centre once or twice a month for check-ins with your physician and your care team.

Continuous Ambulatory Peritoneal Dialysis (CAPD)
With CAPD, dialysis takes place continuously. Dialysis solution is put into and taken out of the body via manual exchanges. Typically, three to five exchanges are done per day in a clean environment - at home, at work or while travelling. After a consultation with your physician, the exchanges can also take place in a suitable room at your workplace, for example. During dialysis, you are not connected to any machine, so you are able to move around during the treatment.
How to perform a bag exchange step-by-step
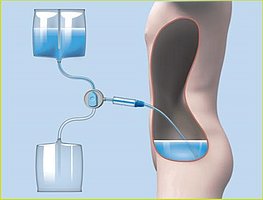
First step
The dialysis solution is passed through the catheter into the abdominal cavity.

Second step
The dialysis solution remains in the abdominal cavity for several hours. Waste products and excess body water are pulled into your abdomen.
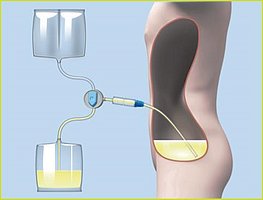
Third step
After a predetermined time, the dialysis solution is drained from the abdominal cavity and replaced with fresh solution.
After applying hygiene measures, you connect the set of CAPD plastic bags filled with dialysis solution to your catheter. The CAPD set typically consists of two bags, one empty waste bag and one bag filled with 2-2.5 litres of cleansing fluid, or dialysis solution. You drain the used dialysis solution through your catheter, which takes about 20 minutes. After draining the used fluids, flush the catheter with a small amount of fresh dialysate.
Now you can fill your abdominal cavity with the fresh dialysis solution. After hanging the plastic bag on the infusion pole at shoulder level, gravity pulls the fluid into your abdomen. This process is called filling and takes about 10 minutes. You can then disconnect the set and cap your catheter.
The whole process, which consists of the three steps - filling, dwelling and draining - is called a bag exchange. This process takes about 30 minutes and is typically done three to five times a day. Some patients prefer to do the bag exchanges before or after mealtime or at bedtime. All the necessary steps are taught and explained to you in advance during a training session.
The dialysis solution remains in your abdominal cavity for several hours. This is called dwelling. During this dwell time, which is the time between two exchanges, waste products and extra fluid are removed from your blood through the peritoneum into the dialysis solution, which is removed from the body at the next bag exchange.
Automated Peritoneal Dialysis (APD)
For APD, the bag is exchanged with an automated process using a portable machine called a cycler. The treatment is different for each patient and is adapted to your personal needs. Your physician will determine the number of bag exchanges and the length of dwell time. Your physician will determine the number of exchanges required along with different amounts of dialysis solution at different times. You will learn how to operate the cycler as part of your dialysis training from your unit.
As a PD patient, you will learn to carry out your therapy independently at home. This comes with a certain degree of personal responsibility. However, dialysis at home does not mean that you are alone! If you have any questions or need more support, you can contact your care team.
Please be mindful that there are pros and cons to all treatment options and PD therapy is not always trouble free. A third of all PD patients encounter repeated problems.The biggest challenges people encounter with PD treatment include psychological problems, infections around the exit site, problems with the PD tube such as drainage difficulties and physical problems including cramps, itching or pain. Please consult your HealthCare Professional to discuss your concerns relating to PD further.
Learn about peritoneal dialysis in the following video:

Haemodialysis
During a haemodialysis treatment, your blood is filtered outside of your body through a dialyser, also called a filter or artificial kidney, to remove unwanted waste, toxins and excess body fluids. For the treatment, a specific access to the blood stream (vascular access) needs to be created that is used to access your blood vessels during treatment. There are three main vascular access types: a fistula, graft or catheter. A surgeon will create this access, usually in the arm or sometimes in the leg if it is a fistula or a graft. Catheters are generally inserted into the vessels in your neck. The preferred access for HD is a fistula, which is an access in the arm made by joining your vein and artery in a small surgical procedure and has been shown to have better outcomes compared to a graft or a catheter.
Haemodialysis uses a solution called dialysate to remove unwanted substances from your blood. Different from peritoneal dialysis, there is a special man-made membrane in the dialyser that allows for the cleaning of the blood. This restores your body and provides chemically balanced blood which is then returned to your body.
A typical haemodialysis treatment takes four to five hours and is repeated three times a week. However, the timing, duration and frequency of haemodialysis depend on your medical conditions and lifestyle as well as your insurance coverage.
If you choose in-centre dialysis, you usually have three fixed appointments per week. With this treatment option, the dialysis team will prepare, carry out and monitor the dialysis for you.
Facts about haemodialysis
- The treatment is carried out by trained nurses and physicians.
- Your dialysis is in one place. You do not have to store dialysis machines or materials at home.
- During dialysis, you can read, relax, work on the computer, watch TV, listen to music or do anything else you enjoy.
- You may also want to talk to other dialysis patients. After all, it is good to know that you are not alone in this situation. For many patients, the dialysis treatment is a place to socialise and sometimes strong friendships develop between fellow patients.
Keep in mind:
- Stick closely to your dialysis schedule: usually three appointments per week, four to five hours a day, plus arrival and departure.
- Complete the entire session. Even stopping five minutes early can make dialysis less effective and harm your health.
- In the first few months of therapy, you may still be exhausted and wobbly on your feet after dialysis. If this is the case, ask a family member or friend to bring you to and pick you up from the sessions. Some dialysis centres may also be able to offer support.

Home haemodialysis
If you choose Home Haemodialysis (HHD), you or a caregiver will perform the preparation, implementation and monitoring of the treatment at home. The dialysis machine and the dialysis items are used in a home-based setting. Depending on the device system that you use, your electricity and water supply may need to be adapted. Some dedicated home machines also allow you to travel.
Home haemodialysis works similarly to in-centre haemodialysis, but the treatment procedure is performed in the comfort of your home. Typically, haemodialysis is performed three to four times a week. For home haemodialysis, there may be the flexibility to add additional treatment sessions: frequent home haemodialysis. Frequent home haemodialysis is usually done five to six times a week and also allows you to perform shorter dialysis sessions, depending on the modality you decide together with your physician. Frequent HHD has been shown to provide different benefits to patients, which may improve flexibility and quality of life.
These benefits can be grouped as physical or mental benefits. For frequent HHD, different benefits have been shown, such as typically having the option of a more liberal diet,1 lowered blood pressure2,3 and associated medication reduction,1 and improved survival rates.4,5,6
Additional mental health benefits of frequent HHD have been described. A short, daily haemodialysis session has been shown to improve mental health and lead to fewer depression episodes.
Moreover, if you are working, there may be more flexibility, as the dialysis time is shorter.
Lastly, sleeping disturbances and restlessness in your legs may be lessened.
All those benefits may have a big impact on a patient’s individual situation and well-being. As a result, frequent HHD could be a treatment option. Please talk to your dialysis team if this may also be an option for you as well.
HHD is proposed as a preferable choice for patients who want to continue to work, stay as flexible as possible and perform dialysis in a familiar environment.
Facts about home haemodialysis
- You are more flexible in terms of work, school or other social activities, as you can choose your dialysis times yourself as recommended by your dialysis team, as compared to in-centre HD.
- You stay in the familiar environment of your own home during dialysis and have the possibility to always reach your dialysis team by phone.
- Typically, you can choose your diet more freely if your physician prescribes more frequent dialysis sessions.
- You do not have to leave the house for dialysis, which saves travel time and transportation costs and you do not need to worry about arrival and departure times.
- You may be able to do the HHD completely on your own. You or your care partner insert the needles yourself, which is preferred by some patients.
Keep in mind:
- Generally, in the first weeks, you go through a training phase, together with a partner or a friend whom you trust, if necessary.
- If you have a family member or friend help you with dialysis, this person must be reliable. The person must agree to assist with your HHD or stay with you to monitor the treatment.
- You or your loved one must be ready to prepare for dialysis and clean the equipment afterwards.
- It must be checked whether your water and electricity supplies need to be renovated or converted. Make sure there is someone who can organise this.
- You also need to create some space at home to store materials and equipment.
- If you are frightened of needles, take that point into consideration when making your decision. Talk to your physician about it!
Dialysis in a centre
If you choose in-centre dialysis, you usually have three fixed appointments per week, typically for a four-hour treatment in your dialysis centre. With this treatment option, in general, the dialysis team will prepare, carry out and monitor the dialysis for you.
Learn about haemodialysis in the following video:
Conservative treatment
Depending on your (medical) conditions, dialysis might not prolong or improve the quality of your life and the best option might be to let nature take its course. Regardless of medical conditions, based on individual situations and preferences, some patients decide not to start or also discontinue renal replacement therapy.
You have the option of not receiving renal replacement treatment and life-prolonging treatment at all. The kidney function will then not be replaced and your kidneys will fail, resulting in natural death. Your health care team will still support you and treat your symptoms with medication and, if necessary, give supportive forms of nutrition. Conservative therapy is more about maintaining quality of life.
Your health team will talk with you to help you make an informed and considered decision.
Make a choice
Keeping and going to your appointments and following your treatment plan is critical to your health. Therefore, it is important to choose a therapy that suits your personal situation. Always remember: The return for the time you invest can be a fuller, more active and healthier life.
You have now learned an overview of what treatment options are available. Together with your medical team, you can discuss and decide which of those treatment options would be the most suitable for you.
Read more about making the right decision in the next section.
What is an Adverse Event (AE)
Any untoward medical occurrence in a patient or clinical trial subject administered a medicinal product and which does not necessarily have a causal relationship with this treatment [Dir 2001/20/EC Art 2(m)].
An adverse event can therefore be any unfavourable and unintended sign (e.g. an abnormal laboratory finding), symptom, or disease temporarily associated with the use of a medicinal product, whether or not considered related to the medicinal product (Annex 4 Guideline on good pharmacovigilance practices (GVP) Rev 4).
Reporting Side Effects
If you get any side effects, talk to your Doctor, Pharmacist or Nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
Report an Adverse Event
Adverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Fresenius Medical Care on 01623 445 215 and via medinfo-uk@freseniusmedicalcare.com
Medical Information
Call 01623 445 100 (please choose option 5). Opening times are Monday - Friday 9am - 5pm.
UK/HEMA/FME/0922/0002 – Date of Preparation September 2022.
1 Mucsi I, Hercz G, Uldall R, Ouwendyk M, Francoeur R, Pierratos A. Control of serum phosphate without any phosphate binders in patients treated with nocturnal hemodialysis. Kidney Int. 1998;53(5):1399-1404. doi:10.1046/j.1523-1755.1998.00875.x
2 Culleton BF, Walsh M, Klarenbach SW, et al. Effect of frequent nocturnal hemodialysis vs conventional hemodialysis on left ventricular mass and quality of life: a randomized controlled trial. JAMA. 2007;298(11):1291-1299. doi:10.1001/jama.298.11.1291
3 Chan CT, Shen SX, Picton P, Floras J. Nocturnal home hemodialysis improved baroreflex effectiveness index of end-stagerenal disease patients. J Hypertens. 2008; 26(9):1795-1800. doi: 10.1097/HJH.0b013e328308b7c8
4 Marshall MR, Polkinghorne KR, Kerr PG, Hawley CM, Agar JW, McDonald SP. Intensive Hemodialysis and Mortality Risk in Australian and New Zealand Populations. Am J Kidney Dis. 2016;67(4):617-628. doi:10.1053/j.ajkd.2015.09.025
5 Rydell H, Ivarsson K, Almquist M, Segelmark M, Clyne N. Improved long-term survival with home hemodialysis compared with institutional hemodialysis and peritoneal dialysis: a matched cohort study. BMC Nephrol. 2019;20(1):52.
Published 2019 Feb 13. doi:10.1186/s12882-019-1245-x
6 Marshall MR, Walker RC, Polkinghorne KR, Lynn KL. Survival on home dialysis in New Zealand. PLoS One. 2014;9(5):e96847. Published 2014 May 7. doi:10.1371/ journal.pone.0096847