HighVolumeHDF
Therapy advantages
HighVolumeHDF , with its numerous positive effects on cardiovascular risk factors in dialysis patients, is acknowledged as an effective dialysis treatment modality1, coming closer to the elimination profile of the natural kidney. By achieving high substitution volumes, HighVolumeHDF therapy is credited with more effective elimination of middle molecules. HighVolumeHDF improves patient outcomes and exerts beneficial effects on the cardiovascular risk factors related to dialysis patients:
- Serum ß2-m and phosphate level2, 3, 4
- Inflammatory response5
- Intradialytic haemodynamic stability6
- Anaemia control9
As dialysis patients are becoming increasingly complex in terms of age and their co-morbid status with diabetes, cardiovascular disease and malnutrition, it is important to use a dialysis modality that accounts for the clinical complexity of these patients to improve care.16
HighVolumeHDF
Optimised use of resources with the CorDiax product line
The innovative and highly automated features of the CorDiax product line support nursing staff by optimising daily work flows and improved patient safety. The result is the easy integration of HighVolumeHDF in the daily routine. The preparation of sterile, non-pyrogenic substitution fluid for HighVolumeHDF is based on a double-stage filtration process.
- No extra costs for an additional single-use filter
- No need for ready-made rinse solutions or a waste bag for priming or reinfusion
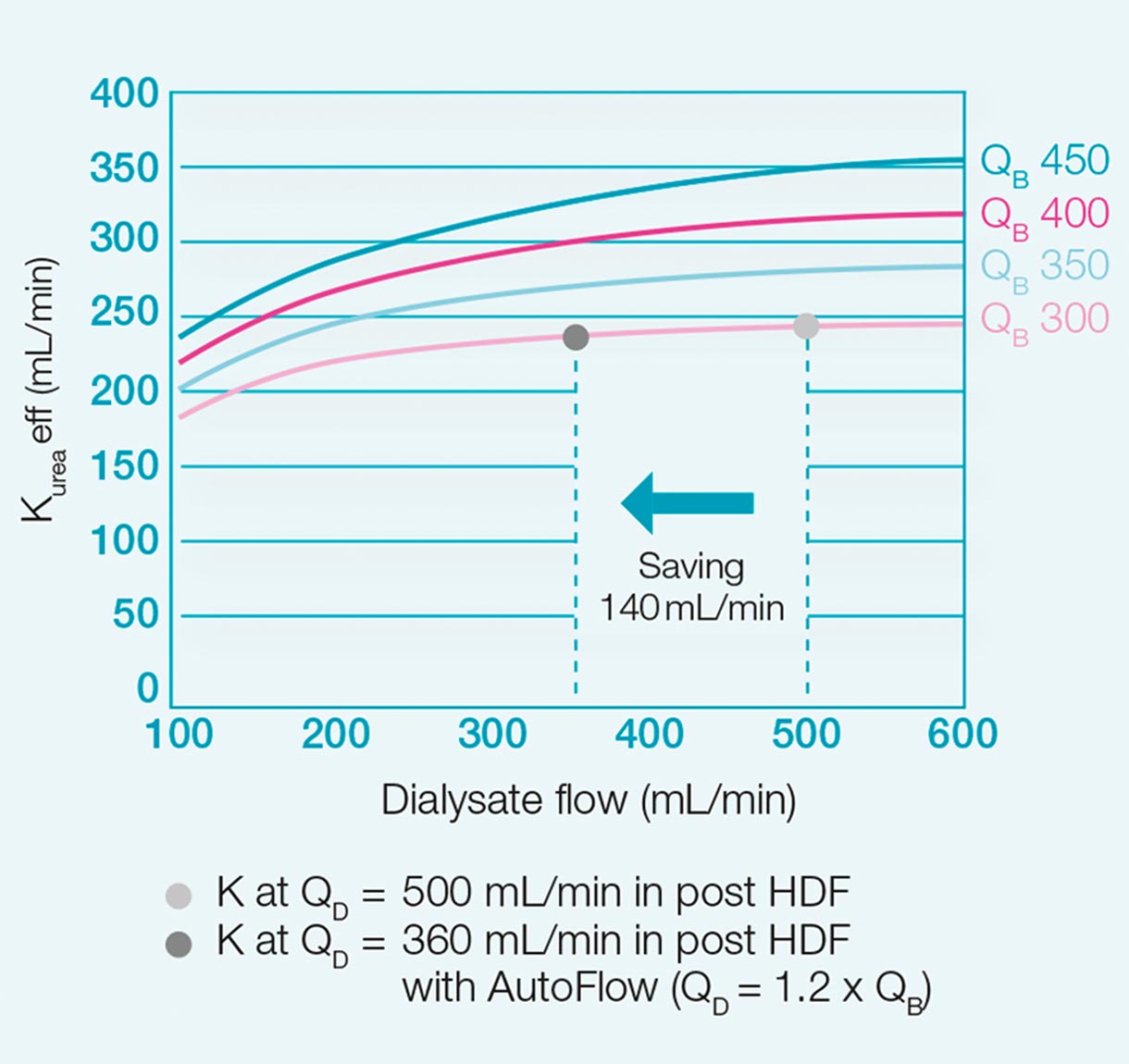
The AutoFlow feature automatically adapts the dialysate flow to the blood flow.
HighVolumeHDF
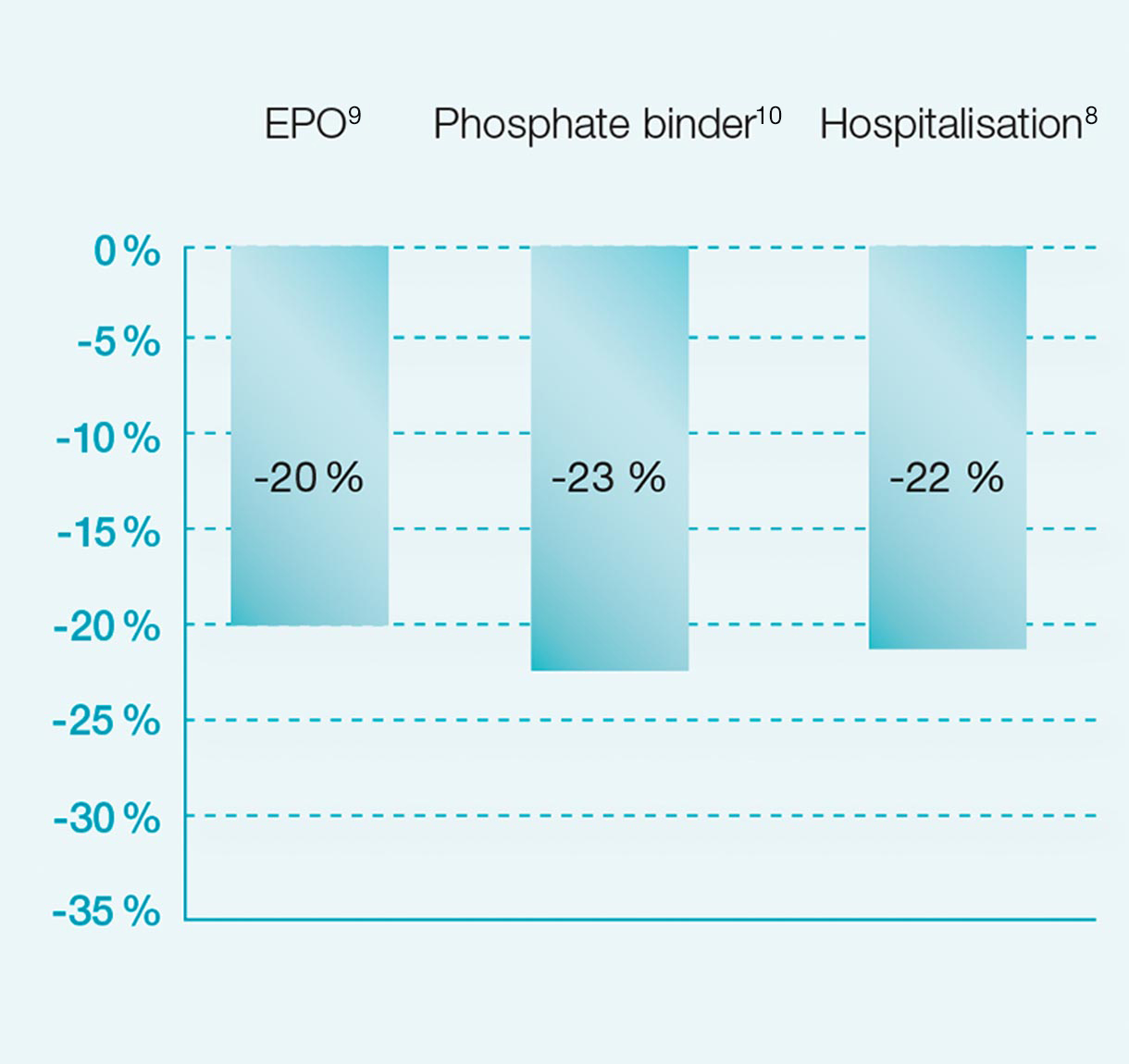
In an economically tight environment, every opportunity to reduce the overall treatment cost should be examined. The amount of EPO1 and phosphate binders4,10 administered to dialysis patients has been shown to be reduced with the application of HDF. Thus, higher quality of care can be provided at a lower medication burden and medication cost.
From promise to proof
Our commitment to achieve the best possible results for every dialysis patient has fuelled our passion for Haemodiafiltration (HDF).
Our belief in HDF is now widely shared across the scientific community and backed by evidence. In recent years, several publications have already confirmed the benefits of HDF.8,9,11-15. The Catalonian high-volume HDF study8 provides accumulating evidence for the benefits of this therapy. Convincing scientific evidence for significantly improved patient outcomes, combined with the simple and reliable use of the 5008 CorDiax, are compelling reasons to switch to HighVolumeHDF now.
That’s why for more than 30 years, Fresenius Medical Care has been developing products for cardioprotective haemodialysis, leading to the CorDiax product line, which perfectly supports the application of HighVolumeHDF therapy.
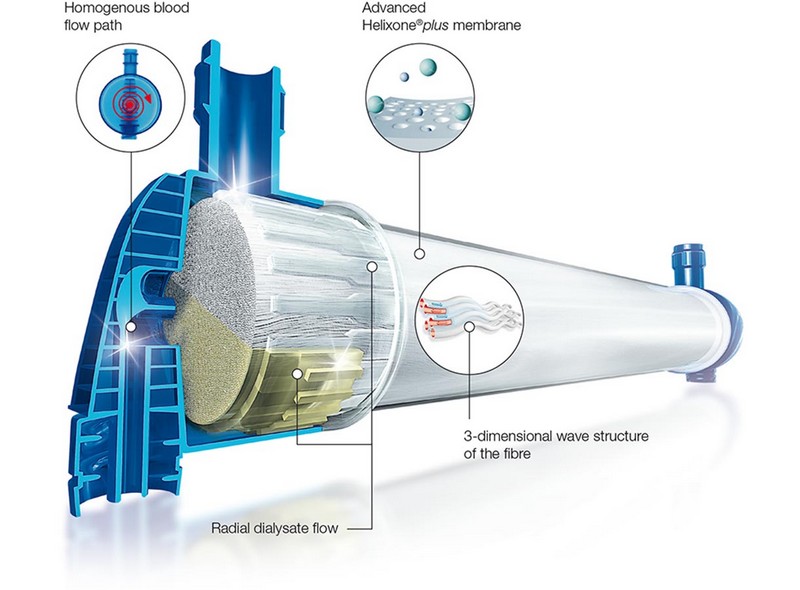
From haemodiafiltration to HighVolumeHDF
Haemodiafiltration (HDF) is a renal replacement technique combining two principles: diffusion and convection. The convective process is based on the ultrafiltration of large amounts of plasma water across the membrane. This allows for the effective removal of larger solutes due to convection in addition to the diffusive transport of small molecules.
To maintain the fluid balance, it is necessary to replace the additional ultrafiltration volume, ideally after the dialyser, which is called post-dilution HDF.
Volume matters in haemodiafiltration
The production of large amounts of substitution volume is no longer a challenge. Today, maximising substitution volume for each patient requires a new therapeutic approach: HighVolumeHDF.
Better patients‘ well-being
| 28% | Risk reduction in incidence of hypotensive episodes (p<0.001) |
|---|
Reduced treatment costs
| 22% | risk reduction in all-cause hospitalisation (p=0.001) |
|---|
Study details8
Products

HighVolumeHDF
The challenges of haemodiafiltration have led us to continuously develop new, innovative products which support the HighVolumeHDF therapy approach. Our long-standing commitment to making HighVolumeHDF available to all patients has resulted in an advanced and highly synergetic portfolio. The result: The 5008S CorDiax and 6008 CAREsystem, in combination with the FX CorDiax HDF haemodiafilter and the Online Purification Cascade (OPC), form an integrated therapy system enhanced by services tailored to support your therapy.

5008S CorDiax and 6008 CAREsystem: HighVolumeHDF as standard
With the new AutoSubplus function of the 5008S CorDiax and the 6008 CAREsystem, HighVolumeHDF has become as simple and reliable as HD, without any need for additional user interaction.

Water Technology: intelligent water quality management
The water technology product line covers all processes for the delivery of the large amounts of substitution fluids required for HighVolumeHDF therapy.
Learn more about water technology
Additional information relating to multiBic or Calrecia can be found in the critical care section of our product information page.
Adverse Events Reporting
Adverse events should be reported. Reporting forms and information can be found at
https://yellowcard.mhra.gov.uk/ or search for MHRA Yellowcard in the Google Play or Apple app store. Adverse events should also be reported to Fresenius Medical Care on 01623 445100.
UK/HEMA/FME/0922/0005 Date of Preparation: November 2022
1 Krick G, Ronco C (eds), Contributions to Nephrology (2011); 175: 93-109.
2 Canaud B., Contributions to Nephrology (2007); 158: 216-224.
3 Penne L. et al., Clinical Journal of the American Society of Nephrology (2010); 5: 80-86.
4 Davenport A., Nephrology Dialysis Transplantation (2010); 25: 897-901.
5 Pedrini L. et al., Nephrology Dialysis Transplantation (2011); 26: 2617-2624.
6 Locatelli F. et al., Journal of the American Society of Nephrology (2010); 21: 1798-1807.
7 Bonforte G. et al., Blood Purification (2002); 20: 357-363.
8 Maduell F. et al., Journal of the American Society of Nephrology (2013); 24: 487-497.
9 Ok E., et al., Nephrology Dialysis Transplantation (2013); 28: 192-202.
10 Pedrini, L. et al., Nephrology Dialysis Transplantation (2011); 26: 2617-2624.
11 Grooteman M.P. et al., Journal of the American Society of Nephrology (2012); 23(6): 1087-96.
12 Canaud B. et al., Kidney International (2006); 69(11): 2087-93.
13 Mostovaya I.M. et al., Seminars in Dialysis (2014); 27(2): 119-127.
14 Peters S.A.E. et al., Nephrology Dialysis Transplantation (2016); 31: 978-984.
15 Basile C. et al., Journal of Nephrology (2017); 30(2): 181-186.
16 Levesque, R., et al., Cost-Effectiveness Analysis of High-Efficiency Hemodiafiltration Versus Low-Flux Hemodialysis Based on the Canadian Arm of the CONTRAST Study. Appl Health Econ Health Policy, 2015. 13(6): p. 647-59.